Colorectal Cancer
Let's start by discussing risk factors for colorectal cancer.
The baseline risk for Americans for developing colorectal cancer in their lifetime is approximately 6%, which is in line with other western societies, but still quite high. This means if no screening tests are done, 6 out of 100 people will get a cancer in their large bowel at sometime in their life.
The most common risk factor is a family history of colon cancer , and if you have one parent who's had a colon colorectal cancer, your risk doubles, which means 12%. If you have two close relatives with colon cancer the risk goes up five to six-fold, so that's somewhere about 30% to 35% risk of getting colon cancer in your lifetime. That's why knowing your family history of colorectal cancer is so important. The other common risk factor is having had a precancerous polyp or a colon or rectal cancer yourself in the recent past.
What is the role - if any - of diet in colorectal cancer?
There is general agreement that our western-type diet, high in animal fats and red meat and relatively low in fruits
>
and vegetables, is a major predisposing factor to colon and rectal cancer. This is very obvious when you look at studies such as those done in native Japanese who eat very differently than Americans, and have a very low percent of colon and rectal cancer. But, when the Japanese migrate to Hawaii or the U.S., their diet changes very quickly and their risk of colon and rectal cancer becomes the same as your average American.
Are most polyps considered precancerous?
There are several different types of polyps that occur in the colon and rectum. Only one type,the adenoma, is known to be precancerous. Adenomas are quite common -- approximately 40% of men over the age of 55 will have at least one. Only one in every 200 adenomas will turn into cancer, but we don't know which ones those will be. On the other hand, all colorectal cancers arise from an adenoma.
"If our current generation of teenagers starts to eat more healthfully, there is every reason to suspect that when they are in their 50s and 60s their incidence of colorectal cancer will be lower than ours."
How should we correct our diets to prevent colon cancer?
There's no evidence that short-term diet changes can reverse the tendency for polyps and cancers to form. However, if our current generation of teenagers starts to eat more healthfully, there is every reason to suspect that when they are in their 50s and 60s their incidence of colorectal cancer will be lower than ours.
Is some type of follow-up treatment in order following removal of one or more adenomas?
Yes. The risk of having more adenomas in the future, after removal of one, depends on the size and the number and the microscopic appearance of the first adenomas. Patients with more than three adenomas are at high risk of developing others and follow-up is quite short. We would recommend repeat colonoscopy one to two years later. Follow-up after removal of large adenomas is also quite short to make sure that the polyp has been completely removed.
It is known that colonoscopy will miss a significant number of adenomas. The smaller the adenoma the greater the risk of it being missed at colonoscopy; therefore, we always schedule follow-up between 3 and 5 years so that if an adenoma was missed at the original examination, it doesn't have a chance to grow too big or become malignant before it is detected.
Is there a correlation between having gastritis and colon cancer? What about Crohn's or IBS or IBD? Are any of these linked to colon cancer?
 There is no association between gastritis and irritable bowel syndrome and colon cancer. Patients with longstanding ulcerative colitis and Crohn's colitis, are at increased risk of developing colon or rectal cancer. Once the colitis has been present for 7 to 8 years, we recommend regular colonoscopies with biopsies to detect precancerous changes in the lining of the colon.
There is no association between gastritis and irritable bowel syndrome and colon cancer. Patients with longstanding ulcerative colitis and Crohn's colitis, are at increased risk of developing colon or rectal cancer. Once the colitis has been present for 7 to 8 years, we recommend regular colonoscopies with biopsies to detect precancerous changes in the lining of the colon.
Is it very rare to have colon cancer under the age of 30?
Yes. Less than 2% of colon cancers arise under the age of 40. When a patient has colon or rectal cancer under the age of 50, there is a strong suspicion that the patient may have some sort of inherited predisposition, such as familial adenomatous polyposis or HNPCC (hereditary nonpolyposis colorectal cancer).
Does age play any role in colon cancer risk?
Yes. I quoted a 6% lifetime risk for the average American. This is the average of an ever-increasing risk from very close to zero at birth to the highest point in the 80s and 90s. The longer you live the higher the risk of colon and rectal cancer. The risk is very low until age 40 and then increases gradually until age 50 and then becomes much higher with each decade.
If you are diagnosed young is there any increase of risk of it returning later in life?
Yes, for two reasons.
- If there is an inherited form of colorectal cancer, there is a much higher chance of developing another cancer later in life. The surgery designed for these syndromes usually involve removal of the entire colon, just for this reason.
- Outside of hereditary syndromes, a young person with a colon or rectal cancer obviously has something about them that has made the cancer arise early. In other words, they're prone to get them. If their colon is able to produce one cancer, it is probable that it will produce another.
"Only about 4% of all colorectal cancers occur because of an inherited genetic mutation."
Are all polyps removed in colonoscopy submitted to lab analysis for cancer detection?
We recommend that all polyps on colonoscopy be removed and sent to the lab for analysis because you cannot tell by looking what type of polyp it is.
Some colon polyps do not increase someone's risk of colorectal cancer and do not warrant special follow-up. However, all precancerous colon polyps do increase the risk of getting new precancerous polyps or cancer and require special follow-up.
Are there reliable genetic tests available to determine colon cancer risk?
Only about 4% of all colorectal cancers occur because of an inherited genetic mutation. For patients in families with these inherited genetic mutations, blood tests are very helpful in showing which members of the family are at risk and which are not. For 96% of all colon and rectal cancers genetic blood testing to determine risk is of no help. Sometimes we can look at the genetic makeup of the tumor itself, but this is still largely a research area.
What kind of special follow-up do precancerous colon polyps require?
The number and size of precancerous polyps found on a colonoscopy, in association with the family history of colorectal polyps and cancer, as well as the patient's previous history of colorectal polyps and cancer, dictate the interval for the next colonoscopy.
Generally, if one to two small (less than one centimeter) adenomas are removed, and the individual has no other risk factors, the next colonoscopy should be in five years. If more than two or larger (greater and equal to 10 millimeters) polyps are removed, the follow-up is generally in three years. However, your doctor may recommend a longer or shorter interval based on the quality of the colonic preparation and other risk factors.
If one or more years generally separate colonoscopies, is it safe to assume that polyps grow very slowly?
It's presumed the development of polyps takes about five years and roughly another five years for them to turn into cancer.
Are you able to determine how long a cancerous tumor has been present? Do colon cancer tumors grow at a fixed rate?
Colon cancer tumor growth rate is very variable. You cannot tell how long a tumor has been present by its size or degree of invasion. The reason is that the growth and spread of a colon cancer depends partly on the aggressiveness of the cancer itself and partly on the ability of the patient's body defenses to contain them. The stage at which a colon cancer presents is, therefore, the result of these two factors. Each patient is different.
Does drinking alcohol increase your risk of getting colon cancer?
There is data suggesting excessive alcohol may lead to colon polyps and cancer. However, recent data shows that drinking alcohol in modest amounts may prevent colon polyps and cancer.
The best approach to colon cancer prevention is a healthy and moderate diet, including fruits and vegetables, low fats and red meats, modest alcohol intake, a reasonable body weight and enhanced activity level.
With gastric bypass surgery becoming more common these days, are you seeing an increase in colon issues as a result?
Gastric bypass surgery, as well as hiatal surgery, may predispose to the development of gastrointestinal symptoms. There is no evidence to suggest that gastric bypass surgery is associated with colorectal polyps and cancer.
"Colonoscopy is usually the preferred screening test."
Let's talk about testing.
There are screening tests, which are used in people without symptoms to prevent cancer by finding and removing polyps or to detect cancer at an early (asymptomatic) stage. There is also another group of tests, which are often the same as used for screening, that are used in symptomatic patients to diagnose an existing cancer.
The most common test used to diagnose colon symptoms that suggests a cancer may be present is colonoscopy. Colonoscopy is also the most accurate screening test for colon and rectal cancer, although its use as a screening test is limited by its expense, the perceived discomfort associated with it and its relative lack of availability.
Other screening tests include fecal occult blood, flexible sigmoidoscopy and barium enema.
New screening tests still under investigation include virtual colonoscopy and genetic testing of DNA in the stool.
The virtual colonoscopy - is it as accurate as the real thing?
Virtual colonoscopy is a novel technique to screen the colon for colon polyps and cancer. Currently it is considered a research tool, and not approved by any major medical societies or reimbursed by insurance.
The majority of studies looking at the accuracy of colonoscopy versus virtual colonoscopy show that virtual colonoscopy is not as accurate. With innovations in software and other imaging techniques, the potential for virtual colonoscopy to be standardly as accurate as colonoscopy is possible.
I read recently that fecal occult blood tests aren't much use because many doctor offices aren't doing them right. Could you comment?
Fecal occult blood testing has been shown in the most stringent of study designs in large populations to decrease colon cancer mortality by up to 33%. However, the accuracy of colonoscopy is much greater than fecal occult blood testing. Colonoscopy is usually the preferred screening test.
If fecal occult blood testing is the strategy used by an individual, it should be done on a yearly basis with the use of three individual cards on a specified diet. If fecal occult blood testing is obtained by a finger examination in the doctor's office, and negative, it should be followed up with the fecal occult blood testing cards done at home as recommended. If the fecal occult blood test is positive on a finger examination, a colonoscopy is indicated, not retesting for fecal occult blood.
What is involved in getting a colonoscopy?
In general, a referral for colonoscopy from the primary physician is required. This is made usually to a gastroenterologist who will usually want to see the patient in consultation first before scheduling the examination. In some areas of the country "open access" colonoscopies are used. This means the family physician can schedule the colonoscopy without seeing the gastroenterologist.
It is essential the colon be completely clean for colonoscopy to have the best chance of finding anything significant and for the patient to have the most comfortable experience possible.
There are four alternatives for cleaning the colon:
- The first is to drink a gallon of slightly salty liquid which flushes the colon out. The advantage of the gallon preparation is that no fluid is absorbed or lost from the body. The disadvantage is that many people find that a gallon is a lot to drink, even spaced out over two hours.
- The second most common bowel preparation is with two small glasses of sodium phosphate (Fleet's). This is much less to drink, although it tastes extremely bad and it is advised to put it in ginger ale to help with the taste. It cleans the colon very well but patients lose fluids and electrolytes. Patients whose kidney or cardiac function is impaired or who are taking water pills (diuretics) should not have Fleet's phospho-soda prep.
- The third option is by taking Fleet's phospho-soda tablets (Viscol). Generally four tablets are taken every 15 minutes the evening before the procedure for a total of 20 tablets and the next morning four tablets are taken twice about three hours before you leave for your procedure.
- The fourth alternative is to take a half a gallon of the salty solution preceded by four laxative tablets.
My primary reason for avoiding a colonoscopy is my adverse reaction to the enema requirement prior to such an exam. Enemas make me tired from being up all night, sore and worn out. I would most sincerely appreciate your suggestions on how I can remedy to this situation.
There are a variety of preparations, none of which include an enema. If patients are completely intolerant to the prep, a three-day liquid diet is occasionally used.
- The only way to cure colon cancer is to remove it.
Is Versed the sedative of choice for most colonoscopies?
The general approach to performing colonoscopy includes conscious sedation. Conscious sedation is sedation given through an IV and generally consists of Demerol or fentanyl with a medication like Versed or Valium.
How long does the procedure take? How soon can you get results?
The procedure takes approximately 15 to 30 minutes and patients are given a report of the findings on the examination immediately. Results sent to the lab often get returned to the physician within a week's time.
If colon cancer is diagnosed, what treatment options does a patient have?
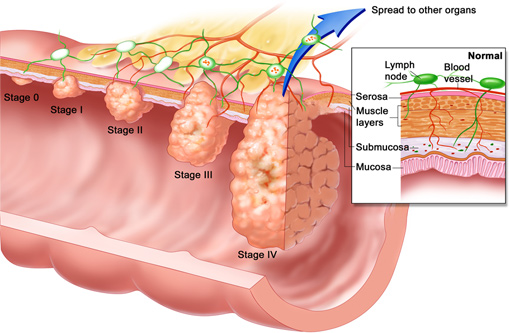
The only way to cure colon cancer is to remove it. This can sometimes be done through the colonoscope if there is a very small cancer that is part of a larger polyp. Usually, however, removal of the cancer requires removal of approximately 10 inches of colon around the cancer, along with the tissues containing the lymph glands, arteries and veins relating to that segment of colon. If the cancer has already spread to the lymph glands when it is removed (stage 3) then chemotherapy is usually recommended. If the cancer has spread to another organ (such as the liver) then cure is very unlikely, unless spread is very slight.
If you don't find the tumor until it is a stage 3 does that mean it is an aggressive tumor or has been there for a long time?
The stage of a tumor bears little relation to the time it has been there. However, a stage 3 is an aggressive tumor and the likelihood of cure is less likely than a stage 1 or 2 cancer.
Do the latest chemotherapy drugs lessen the adverse side effects of treatment?
Every chemotherapy drug has its own list of side effects, and currently there are several choices that patients and their oncologists can make. In general, the more aggressive the chemotherapy the higher the risk of side effects.
For the usual adjuvant (or preventive) chemotherapy with 5FU, Xeloda, side effects are minimal. When other drugs, such as irinotecan or oxaliplatin are used, side effects increase significantly.
What do you exactly mean by "cure"?
Cure generally refers to the avoidance of having recurrent colorectal cancer five years after it's been removed. In general, the survival rates are based on the colon tumor stage. For stage 1 colon cancer, the five-year survival rate or chance of cure is greater than 90%, and in some institutions, it's greater than 95%. The chance of cure or survival gets progressively worse with increasing stage so that it is 80% for stage 2, 40% to 60% for stage 3, and approximately 10% for stage 4.
How can family members assist/comfort a patient undergoing chemotherapy?
Receiving the diagnosis of cancer yourself or as a relative or good friend is often shocking and devastating. Making yourself available for emotional support of your loved ones can make this time easier on the individual with cancer. Many support groups are available for individuals affected with colorectal cancer and for their loved ones.
Does the gastroenterologist direct the treatment, or is he/she out of the picture once cancer has been diagnosed?
Once cancer has been diagnosed the treatment of the cancer, if surgery is required, is usually undertaken by the colorectal surgeon. If chemotherapy or radiation therapy is required, that care is directed by a cancer physician who is called an oncologist. However, if follow-up colonoscopies are required to check the colon for recurrent tumors, the gastroenterologist often provides those examinations.
"Make sure that you and all of your friends and family get screened for colorectal cancer so we can prevent this dreadful disease."
I'll be asking my doctor soon for a colonoscopy (my mom was recently diagnosed with Stage 4 colon cancer). Meanwhile, what over-the-counter product (type) is best to flush the colon on a regular basis to reduce the likelihood of polyp formation?
It's excellent that you are getting your colonoscopy performed because you are at an increased risk of colorectal cancer based on your mother's recent diagnosis of colorectal cancer. All individuals, even without symptoms, over the age of 49 should have screening colonoscopy.
There is no evidence that cleansing the colon on a regular basis will prevent polyps or cancer in the colon. The known risk factors for polyps and cancer include many things we cannot change, like our genetic makeup and age, or associated inflammatory conditions in the intestine like Crohn's disease or ulcerative colitis. The risk factors that are under our control that could minimize the risk of colon polyps and cancer include avoidance of smoking, maintaining a normal weight, having daily physical activity, and a diet that is high in fruits, vegetables, and fiber intake while avoiding fats and processed meats.
The inside of the colon is lined with mucus-secreting cells and appears pink and glistening when viewed. Many individuals are under the impression that the colon gets clogged with waste matter and requires cleansing frequently for good health. This is untrue.
My mother died at the age of 47. She had cervical cancer and colon cancer, but the colon cancer was "secondary" and an off shoot of the original cancer. So, does that put me at increased risk for colon cancer given that hers was a secondary cancer?
There are a few colorectal cancer syndromes that include primary cancers in multiple places. It sounds as if your mother's cancer may have extended from the female organs into the adjacent colon by local growth. However, if your mother had a confirmed colon cancer (not cervical cancer extending into the colon) you are at increased risk of colorectal cancer and should have a colonoscopy ten years younger than the age of your mother's colon cancer detection or at the age of 40 if your mother was over age 60.
I may have to skip my last two treatments of 5-FU and oxaliplatin because of elevated liver enzyme level. Are there any consequences for not getting my last two treatments and how is elevated liver enzyme levels caused?
Medications used to treat a variety of physical conditions are metabolized in the liver. These medications can have direct effects on the liver cells which may include inflammation of the liver which results in elevated liver enzymes. There are other mechanisms for liver enzyme abnormalities related to medications and they are somewhat complex.
The risks and benefits of ceasing your chemotherapy needs to be discussed with the treating physician and weighed to ensure you come to an informed decision about the next course of care.
We are almost out of time. Before we wrap things up for today, do you have any final words for us?
After this chat you know how important it is to prevent colorectal cancer, which kills nearly 50,000 of us each year. Make sure that you and all of your friends and family get screened for colorectal cancer so we can prevent this dreadful disease

